Need help with Kansas Medicaid? Make an appointment with KAN?
Who qualifies for Kansas Medicaid?
Unfortunately, Kansas has some of the most strict Medicaid rules in the country. Adults without children who are not disabled usually do not qualify for Medicaid, regardless of income. Even for adults with children, the income guidelines are so low that most adults do not qualify for Kansas Medicaid.
There are several Medicaid programs for different Kansas residents.
In order to get Medicaid, you must be a Kansan who is one of the following and meet certain income limits:
a child under the age of 19
a pregnant person
an adult with children or a caretaker
elderly or disabled
Medicaid Income Guidelines for…
Pregnant People
Household of 2 = $0 - $2,810
Household of 3 = $0 - $3,543
Household of 4 = $0 - $4,275
Household of 5 = $0 - $5,007
Household of 6 = $0 - $5,740
Children under 19
Household of 2 = $0 - $4,1,91
Household of 3 = $0 - $5,283
Household of 4 = $0 - $6,375
Household of 5 = $0 - $7,467
Household of 6 = $0 - $8,560
Parents and Caregivers
Household of 2 = $0 - $624
Household of 3 = $0 - $787
Household of 4 = $0 - $950
Household of 5 = $0 - $1,113
Household of 6 = $0 - $1,276
*all income guidelines as of 04/23
Medicaid health insurance is only for people who are US citizens or meet immigration guidelines. Folks without social security numbers can not get Medicaid. They can, however, apply for family members like children. Social security numbers are NOT required for people applying on behalf of family members.
The Medicaid Gap
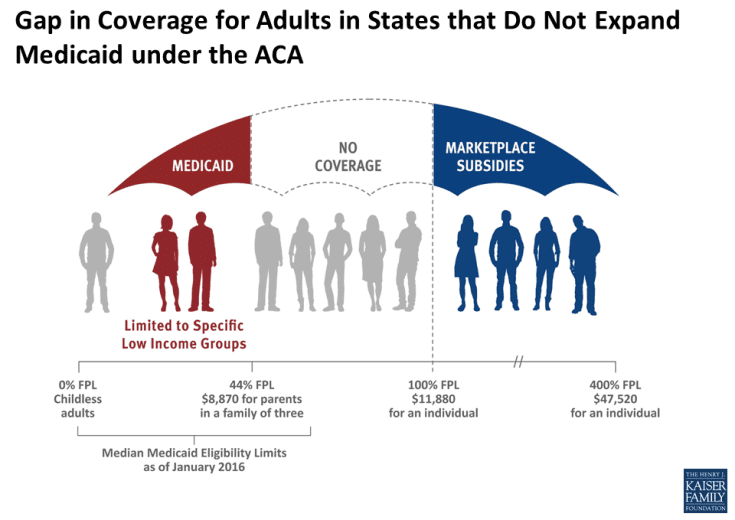
One of the key parts of the Affordable Care Act (ACA) is the expansion of Medicaid eligibility to nearly all low-income individuals with incomes at or below 138% of poverty (see chart below). While the Medicaid expansion was intended to be national, the June 2012 Supreme Court ruling made it optional for states. Kansas chose not to expand Medicaid.
Because the ACA envisioned low-income people receiving coverage through Medicaid, it does not provide financial assistance to people below poverty in the Marketplace. As a result, many adults in Kansas fall into a “coverage gap” of having incomes too high for Medicaid eligibility but too low for financial assistance in the Marketplace.
If you fall in the Medicaid gap, reach out to KAN to tell your story so we can advocate getting Medicaid Expansion in Kansas.
Other Kansas Medicaid Programs
Children’s Health Insurance Program (CHIP)
Children from families with incomes on the higher end of eligibility may need to pay a small premium every month. This is called the Children’s Health Insurance Program (CHIP).
If the family’s income is at the KanCare CHIP level, additional rules apply.
A premium between $20 and $50 is required for families with higher incomes.
Medicare Savings Plans
This Medicaid program pays Medicare out-of-pocket expenses. This includes premiums and co-payments. A single person must have assets below $9,430 and a couple must have assets below $14,130 for QMB and LMB. There are two different programs:
Qualified Medicare Beneficiary (QMB): Single persons must have a monthly income below $1,255. Couples must have a monthly income below $1,704. This program pays for the Medicare Part B premium. It also pays Medicare co-pays and deductibles.
Low Income Medicare Beneficiary (LMB) and Expanded Low Income Medicare Beneficiary (ELMB): For LMB, single persons must have a monthly income below $1,506, and for couples below $2,044. For ELMB, single persons must have a monthly income below $1,695, and for couples below $2,300. These programs pay for the Medicare Part B premium.
Other Medicaid programs
MediKan: This is a Medicaid plan for persons with disabilities. Most persons have a pending application with Social Security. Persons may receive MediKan for 12 months. MediKan has limited services. Services do include prescription drugs and medical.
SOBRA: This plan is for persons who do not meet citizenship rules and cannot receive Medicaid benefits. It covers life-threatening emergency care costs and birth/delivery services. The program may also cover families with children, elders, and persons with disabilities. Persons must meet income and asset rules to qualify.
Breast and Cervical Cancer: This Medicaid plan is for persons with breast or cervical cancer. The Early Detection Works program must diagnose the condition. The Early Detection Works program offers free breast and cervical cancer screening to some women ages 40-65. For information on the Early Detection Works program, call toll-free, 1-877-277- 1368. A nurse with the Early Detection Works program will help women apply for the program.
Inpatient Tuberculosis Care: This Medicaid plan covers tuberculosis treatment in a hospital setting.
Long Term Care Options
Nursing Facility Coverage: This Medicaid plan is for persons in a nursing home or similar facility. Single persons must have assets below $2000. KanCare will not count the value of the home if the person intends to return home. There may be penalties when assets are sold or given away. KanCare looks at sales and gifts within the past five years. Persons with an income of more than $62 a month help pay for their care. Allowance for private health insurance may be given
Home and Community-Based Services (HCBS): This Medicaid program offers services in the community instead of in the nursing home. HCBS is much like nursing home health care coverage. Persons must have a medical need for special care. There must be an open space in the HCBS program. The asset limit is $2000 for single persons. People on HCBS must also share in the cost of care. Persons with an income of more than $747.00 a month help pay for their care. Allowance for private health insurance may be given.
Program of All-Inclusive Care for the Elderly (PACE): This is a program for persons ages 55 and older. They must live in Dickinson, Douglas, Ellsworth, Harvey, Jackson, Jefferson, Lincoln, Lyon, Marion, Marshall, McPherson, Nemaha, Osage, Ottawa, Reno, Rice, Saline, Sedgwick, Shawnee, Pottawatomie, Wabaunsee, or Wyandotte Counties. It provides long-term care through a managed care network. This only covers the medical expenses of providers in the managed care network. For people living in the community, the HCBS rules apply. For people who move to a nursing facility, the nursing facility rules apply.